|
 |
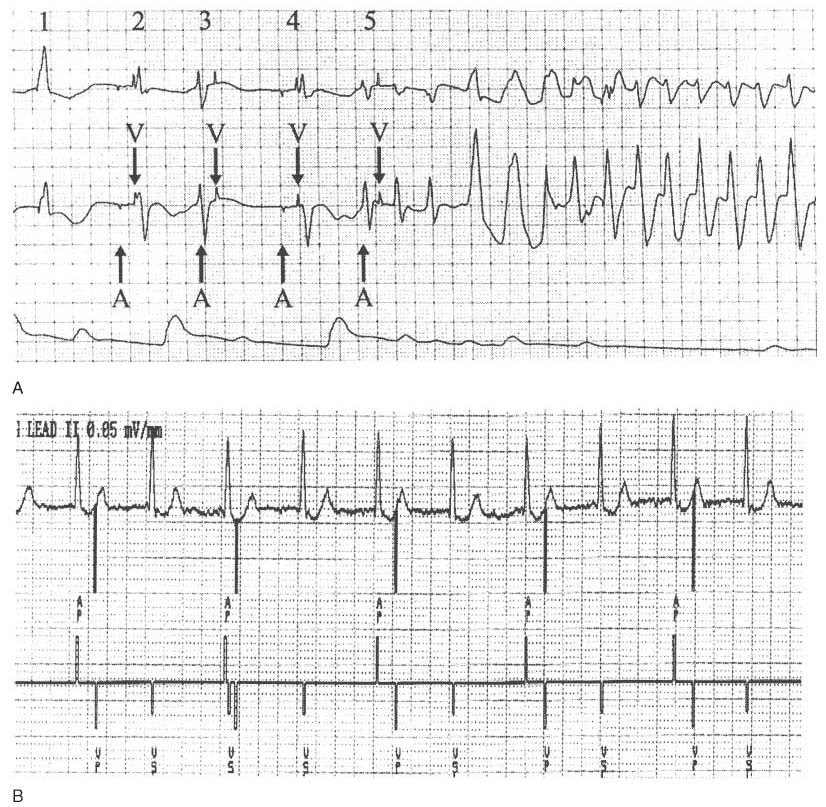
Figure 35-6
Normal dual chamber pacemaker timing can produce R-on-T
pacing. A, This strip demonstrates functional ventricular
undersensing of a premature ventricular contraction (PVC) with a resultant R-on-T
pace leading to torsades de pointes. This patient had a dual chamber pacemaker in
the DDD mode with a programmed lower rate of 70 beats/min (R-R interval is 857 msec)
and an atrioventricular delay of 200 msec. With these parameters, the pacemaker
paces the atrium at 657 msec after any previous ventricular event. Atrial pacing
(A) and ventricular pacing (V) are indicated. The top tracing
is electrocardiographic (ECG) lead II, the middle tracing
is ECG lead V5, and the bottom tracing is the invasive
arterial blood pressure. Approximately 660 msec after the first QRS (1) on the strip
(which was adequately sensed by the pacemaker), an atrial stimulus is emitted. At
200 msec after this atrial pace, a ventricular stimulus is emitted, appearing to
depolarize the ventricle (2). About 660 msec later (3), the patient had a PVC.
Because the pacemaker was preparing to emit the atrial stimulus, it had disabled
its ventricular sensing element and failed to sense this PVC (i.e., functional undersensing).
At 200 msec after the atrial stimulus, no ventricular event had been sensed, and
the pacemaker emitted a ventricular stimulus on the T wave. Because the ventricle
was in a refractory period from the PVC, there was no depolarization of the ventricle
(i.e., functional noncapture). At 660 msec from this attempted ventricular pacing,
the pacemaker again paces the atrium (4), and it appears that the next ventricular
pacing impulse captures the ventricle. At (5), there is a repeat of the events at
(3); the pacemaker disabled its sensing elements in preparation to pace the atrium
and failed to detect the PVC. This time, however, the ventricular pace on the T
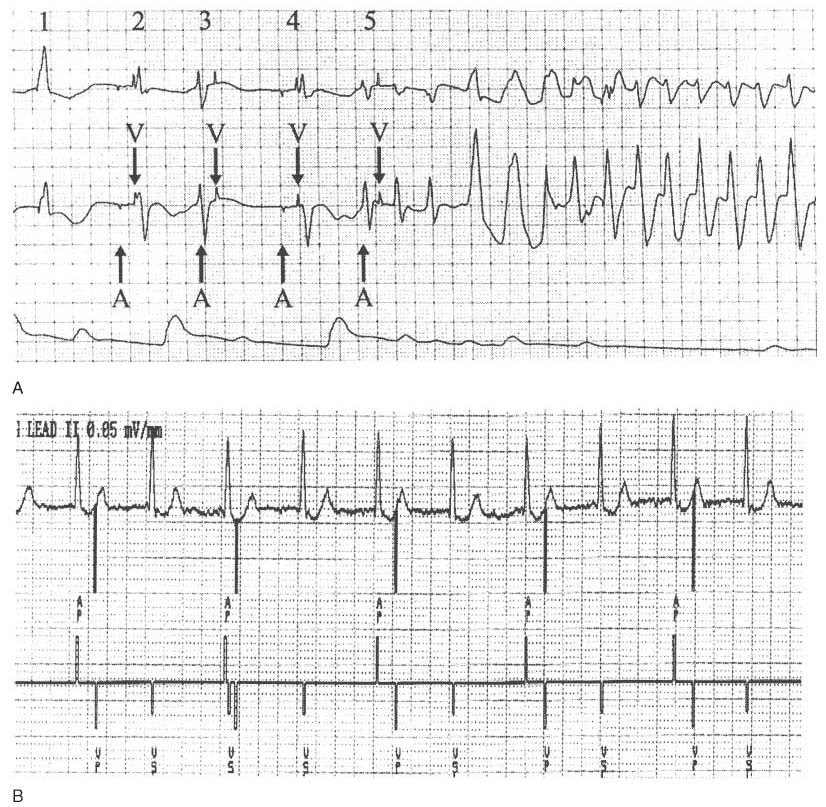
wave produced torsades de pointes. B, This strip
was obtained from a Medtronic programmer during interrogation of a Kappa 700 dual-chamber
pacemaker. The top tracing is ECG lead II, and the
bottom tracing is the marker channel, which shows
the pacemaker's interpretation of events. This pacemaker was programmed to the DDD
mode with a lower rate of 60 beats/min. The atrioventricular (AV) delay was 200
msec. As a result, after any ventricular event, the pacemaker will emit an atrial
pulse at 800 msec if no intervening atrial or ventricular event takes place. This
patient had a junctional rhythm at 75 beats/min (corresponding to an R-R interval
of 800 msec), and the pacemaker emitted an atrial pulse just as the junctional event
occurred. Because the pacemaker disables its ventricular sensing element when emitting
the atrial pulse, it failed to detect the ventricular event and emitted the ventricular
pulse 200 msec later, falling on the T wave. This inappropriate pacing takes place
every other cycle, because every other junctional event is sensed about 600 msec
after the previous ventricular pace. Decreasing the AV delay decreases the likelihood
of pacing during the vulnerable period of the ventricle. Atrial pace (AP), ventricular
pace (VP), and ventricular sensed event (VS) are indicated. The third complex deserves
comment. The pacemaker sensed this ventricular event as it re-enabled its sensing
element, and the pacemaker could not tell whether the sensed event was a true ventricular
depolarization or an echo of the atrial pace (called far-field oversensing). When
a signal from the ventricle is sensed within 30 to 90 msec after an atrial pace,
many pacemakers immediately emit a ventricular pacing stimulus. Called a ventricular
safety pace, this pacing stimulus is designed to protect the patient from
inappropriate sensing of the atrial signal by the ventricular channel, which would
then inhibit the ventricular output. The safety pace is emitted at 110 msec to prevent
R-on-T pacing. This feature is also called nonphysiologic AV
delay by some manufacturers. R-on-T pacing can be appropriate (but not
ideal) behavior of a DDD or DDI pacemaker in the setting of PVCs or a junctional
rhythm. It can also be seen with atrial or ventricular undersensing.
 |